Why hospitals are losing the LOS battle, and how AI is helping to change the outcome
Blog
Introduction: the persistent challenge of LOS
Hospitals across the United States continue to struggle with LOS because discharge delays, capacity limits and day-to-day flow pressures make it difficult to move patients through the system efficiently. Both the American Hospital Association (AHA) and the Institute for Healthcare Improvement (IHI) highlight how these bottlenecks create avoidable extensions in care that strain teams and limit capacity. Under the IPPS fixed-payment model, every unnecessary inpatient day increases resource use without increasing reimbursement, putting further pressure on margins.
AI clinical surveillance technologies could help address patient flow problems
Clinical deterioration is often preceded by subtle physiological changes that, if not recognized, can progress to more serious outcomes. Yuan et al., noted that traditional scoring systems to predict clinical deterioration, had limitations. This observation prompted them to explore the effectiveness of AI models, to better predict clinical deterioration and, in turn, better outcomes. In their meta-analysis, they found that AI-based early warning models made a measurable difference in clinical outcomes, offering a viable route to reducing LOS, and showing significant associated reductions in in-hospital and 30-day mortality.
Etiometry’s AI platform is helping hospitals today to reduce LOS and ICU LOS.
The Etiometry clinical intelligence platform has multiple FDA-cleared adjunctive risk indices, and, most notably, clinical outcomes data that show how the platform is associated with reduced LOS. The platform integrates with existing EHR systems and bedside monitors, ensuring minimal disruption to current workflows while maximizing data utility.A recent study found that the deployment of the Etiometry Platform was associated with a 20% reduction in postoperative hospital LOS, without impacting key measures of clinical care. In another reported study, application of the Etiometry platform was associated with reductions in ICU LOS of up to 36% in the postoperative phase.
These results help us to understand the significant cost savings available from a reduction in post operative LOS. When risk-adjusted and translated into hospital cost terms, these improvements equate to estimated savings of between $3,336 and $8,671 per patient. With the average inpatient day costing around $2,383 and each additional day of mechanical ventilation adding roughly $1,500, even modest reductions in length of stay can rapidly deliver substantial financial benefit across a hospital’s annual case volume.
Etiometry’s Clinical Outcomes Improvements Translate into Reduced Cost of Care
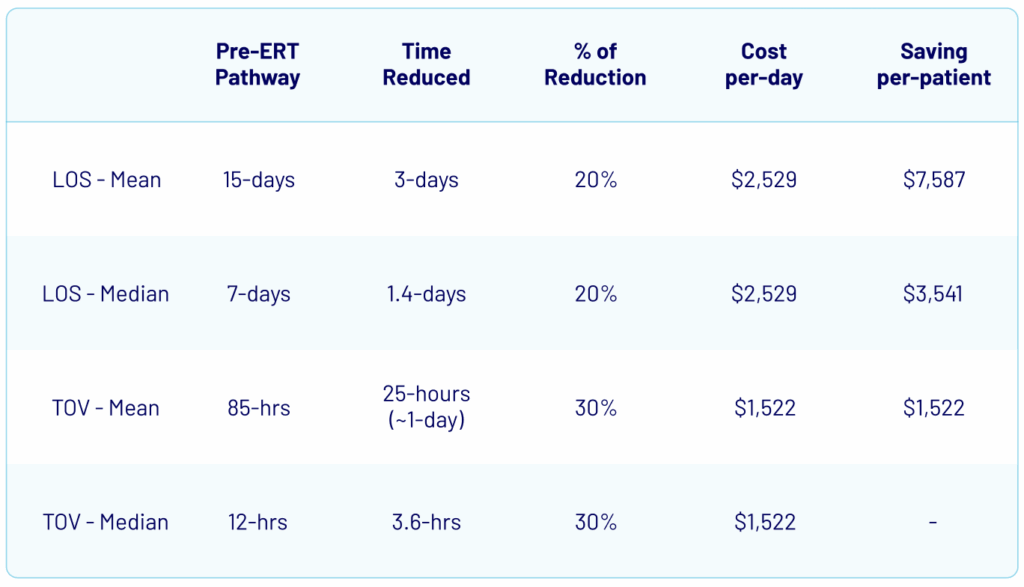
Assumptions:
- Cost per day: $2,383
Source: https://www.statista.com/statistics/630443/inpatient-day-hospital-costs-in-us-by-nonprofit-or-profit/ - Mean incremental cost of mechanical ventilation in intensive care unit patients: $1,522 dollars per-day
Etiometry’s clinical intelligence moves patients through hospitals more efficiently
Etiometry provides FDA‑cleared adjunctive indices and visualization tools that support clinician review and communication related to escalation/de‑escalation discussions in accordance with hospital protocols.
Contact Us
Contact us if you’re seeking to automate the efficient escalation and safe de-escalation of care workflows, or equip your team with AI-based clinical intelligence to enhance outcomes and reduce length of stay.
1.https://bmcmedinformdecismak.biomedcentral.com/articles/10.1186/s12911-025-03048-x
2.Clark M.G., Borasino S., Zaccagni H.J., et al. Automated spontaneous breathing trial performance tool is associated with improved outcomes following pediatric cardiac surgery: A single-center retrospective study from Alabama, USA. Journal of Pediatric Critical Care, 2025;12(1):1-7.
3.The Impact of a Real-Time Physiologic Data Analytic Index on Length of Stay in Neonates Following Surgery for Congenital Heart Disease, Joshua W Salvin, Dimitar Baranov, and Peter C Laussen https://www.ahajournals.org/doi/10.1161/circ.136.suppl_1.20603
4.https://www.statista.com/statistics/630443/inpatient-day-hospital-costs-in-us-by-nonprofit-or-profit/. Mean incremental cost of mechanical ventilation in intensive care unit patients: $1,522 dollars per-day