How We Help
Tap into the Etiometry clinical intelligence platform to:
- Enable proactive and personalized care escalation and de-escalation
- Automate quality improvement for care standardization
- Facilitate the measurement, iteration and optimization of your care delivery processes
- Find significant savings and revenue opportunity
Tighten communications during Handoffs
Enlist the help of Etiometry to tighten your care team communication during shift changes, sign-outs, breaks, patient unit transfers and discharges to a receiving entity or family member. The handoff is often a key criterion for adjudicating quality care delivery —particularly in high acuity areas. Use Etiometry to:
- Validate assumptions or reports of changes in patient condition
- Reduce omission of information
- Establish a baseline for a patient (e.g., a moderately low blood pressure baseline) to prevent over-indexing on one value
- Show the clinical course over time and responsiveness, or lack thereof, to treatment
- Provide a pre-emptive review of a patient prior to a verbal handoff to help clinicians ask the right clarifying questions
- Prioritize patients
- Inform discharge decisions
Gain important insights with Event Reviews
Gain reassurance that the team did all that can be done by learning from the sequelae of events that lead to deterioration, using Etiometry’s:
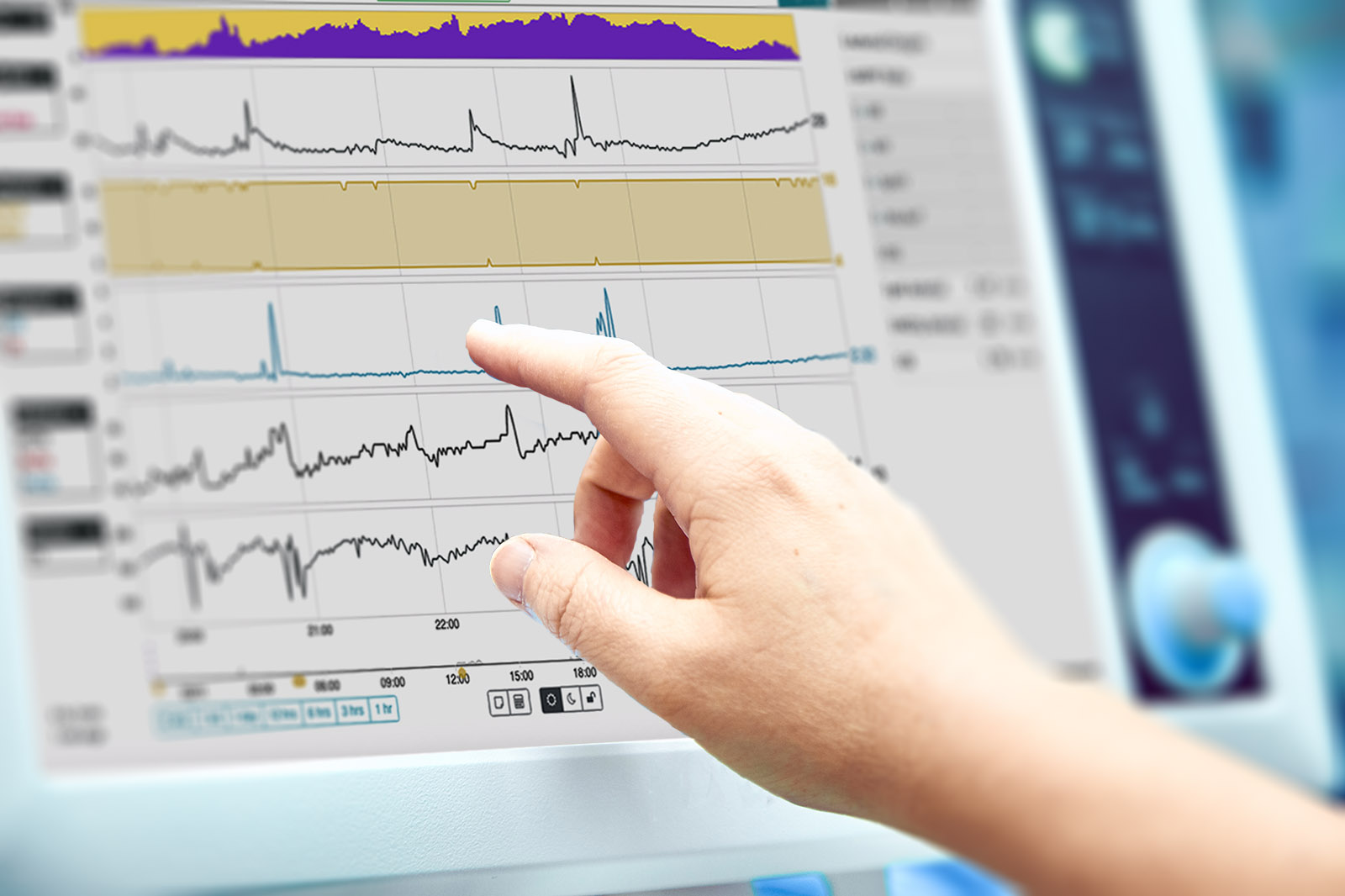
- Longitudinal Patient View (trends over time)
- Holistic Patient View (multiple data sources aggregated into one view)
- Event markers and a sense of time between key events or interventions
Build confidence in newer clinicians
Use the Etiometry platform to communicate the big picture of what is going on with the patient.
Immediate access to aggregated, trended patient data on one Etiometry screen helps alleviate the pressure on newer clinicians to clearly articulate issues that might not have surfaced during physician rounds. Etiometry paints the picture automatically, so any care team member can simply show a visualization of what they are observing.
Spontaneous Breathing Trials (SBTs) or Extubation Readiness Trials (ERTs) using Etiometry’s Clinical Pathway Automation
Know when a patient is ready for an SBT based on pre-determined parameters to reduce exposure to invasive mechanical ventilation and potentially reduce length of stay.
Extended ventilator time may also have system wide consequences related to throughput and reimbursement.
Reduction in ventilation time can reduce length of stay, drives bottom-line savings and could open a bed for another patient.
Clinical data show up to a 22% reduction in ventilation time and 19% reduction in hospital length of stay by utilizing Etiometry’s automated ERT pathway.
Borasino, S. et al. (2023) Automated Extubation Readiness Tool is Associated with Improved Outcomes Following Pediatric Cardiac Surgery. World Congress of Pediatric Cardiology and Cardiac Surgery
Vasoactive Medication Weaning using Etiometry’s Clinical Pathway Automation
Although crucial for hemodynamic management, vasoactive medications carry risks of complications and require close monitoring and individual patient management for appropriate care de-escalation.
Get informed when patients meet weaning criteria with Etiometry’s Clinical Pathway Automation, which continuously scans patient data to determine eligibility to wean based on your unit’s thresholds. A new standardized workflow can lead to earlier recognition of readiness to wean vasoactive support. In fact, there are clinical data showing Etiometry use reduced time on vasoactive medication by 18%. The vasoactive weaning pathway informs data-driven decisions to decrease vasoactive medication exposure.
Salvin, J. et al. (2023) Use of a Risk Analytic Algorithm to Inform Weaning from Vasoactive Medication in Patients Following Pediatric Cardiac Surgery. World Congress of Pediatric Cardiac and Cardiac Surgery.
Support your patient and family education interactions
Help family members understand the complexity or acuity of their loved one and provide them the information they need to make informed decisions in their care, e.g., ICU liberation bundle or end of life care. Etiometry:
- Can help explain the ‘why’ behind clinical decisions
- Shows the longitudinal trend of patient data
- Provides visual cues that are easy to digest and understand (e.g., upward or downward trends)
Clinical Decision Support from the Bedside or Remotely
Understand and communicate the patient condition from anywhere patient data are viewed by the care staff – this includes persistent display at the bedside, a workstation on wheels, a central command center or anywhere you can access your hospital VPN. Etiometry’s web-based platform works with your existing architecture to support your existing workflows.
Etiometry continuously collates data from the EHR, balloon pumps, ventilators, telemetry, arterial lines and any other patient monitoring device, so clinicians can go to one screen for a holistic patient view and note subtle trends.
How can Etiometry help you and your care team?
Clinical and operational uses that are driving standardized and individualized care:
- AKI screening
- Cardiac arrest prevention bundle
- Efficient and safe care escalation and de-escalation
- Discharge decisions
- Extubation
- Fast-track extubation
- Goal directed therapy
- Goal directed perfusion in the OR
- Heart failure screening
- Hospital / System-wide surveillance
- ICU liberation
- Medication decisions
- Remote monitoring
- Step-down unit remote monitoring
- Tele-ICU command center
- Transfusion decisions
- Vasoactive medication weaning
- Care team communication
- Handoffs
- M&Ms / Event reviews
- Nurse-led rounds
- Optimized RN handoff solutions
- OR or ICU handoff solutions
- Prioritizing patients by acuity
- Rounds
- Teaching
- …and more